According to the definition, a geriatric patient is a person over the age of 60, whose body is constantly changing due to the progressive aging process of the body. As time passes, absorption weakens, gastric juice acidity and peristalsis decrease, liver metabolism slows down, kidneys function less well. These are just a few examples of the changes taking place, but everything that happens in the body can affect how we react to the drugs we take. According to statistics, 15-20% of hospitalizations of people over 65 are caused by side effects of medications. The more a patient takes them, the higher the risk of side effects.
Therapeutic chaos
Most seniors are treated by primary care doctors, but they also seek help from various specialists. They go to the doctor because a new problem has arisen that they want to solve. But they go unprepared. They usually don't tell the doctor about their chronic diseases and the medications they are taking. The doctor does not ask or asks very rarely. If he recognizes an ailment, he issues a prescription for another drug and everyone thinks the problem is solved. Are you sure? The consequence of such behavior is so-called therapeutic chaos, which leads, among other things, to seniors taking from three to more than 10 medications a day. Taking eight drugs a day is associated with a 100% occurrence of interactions [1, 2].
One more issue worth mentioning is the drug cascade. This is a concept that refers to the phenomenon of prescribing or self-incorporating new drugs. The drug cascade occurs as a result of the treatment of various conditions by specialist doctors who have not been informed of other drugs used by the patient. The number of drugs used by a senior should be reduced not only because of the possibility of interactions, but also because of improved compliance, which leads to more effective treatment.
Through the eyes of a pharmacologist
Blaming geriatric patients for drug addiction is unjustified, since most of them try to follow their doctors' instructions. Yes, there are elderly people who abuse medications, just as there are people who overeat sweets. When meeting a patient with a doctor, the former is completely defenseless. He takes on faith everything the doctor says and recommends. Most patients do not analyze the specialist's decision, because they are not familiar with medicine and do not know what drug interactions are. They do not inquire how to take the drug and what not to combine it with.
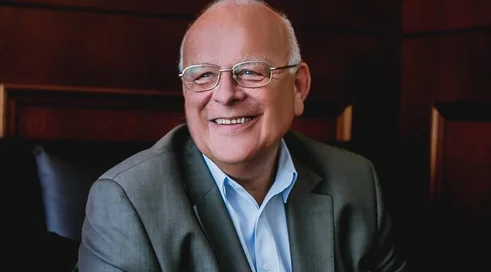
- For a geriatric patient, a professional health care professional is like St. Peter, because he gives hope for a pass to continue living, says Dr. n. pharm. Leszek Borkowski, a clinical pharmacologist at the Mazovian Bródnowski Hospital. - Hence, any carelessness or oversight we make reflects on the geriatric patient. I work as a clinical pharmacologist in a large Warsaw hospital. I deal with patients through the medications they take. As a pharmacist, I don't diagnose or determine first-line therapy. I show up when it is necessary with a multi-disease, or multi-drug patient to swap something with something, recommend a different dosage, frequency, choose medications for exacerbation of chronic renal or liver failure, suggest additional laboratory...
Content locked
To gain access to the complete English section of the Medexpress.pl, kindly reach out to us at english@medexpress.pl.